Research focusing on soft-tissue sarcoma
Sarcomas are mesenchymal tumors arising from the bone or soft tissues and are relatively more common in children and young adults being the cause of 13% of cancer related deaths in patients with up to 19 years of age. They are group of tumors particular challenging to treat due to their high heterogeneity, limited understanding of molecular tumorigenic mechanisms and scarcity of models for translational studies. The aim of the junior research group "soft-tissue sarcoma", which corresponds with the DKFZ group of the same name, is to fill these critical gaps by applying state-of-the-art technologies to understand underlying oncogenic molecular mechanisms, and develop novel in vitro and in vivo sarcoma models. We combine several biochemical, gene editing and genome-wide occupancy techniques to study epigenetic mechanisms deregulated in sarcomas and develop more flexible immunocompetent animal models to support clinical translation. By elucidating mechanisms of cancer pathogenesis we aim to reveal novel therapeutic strategies.
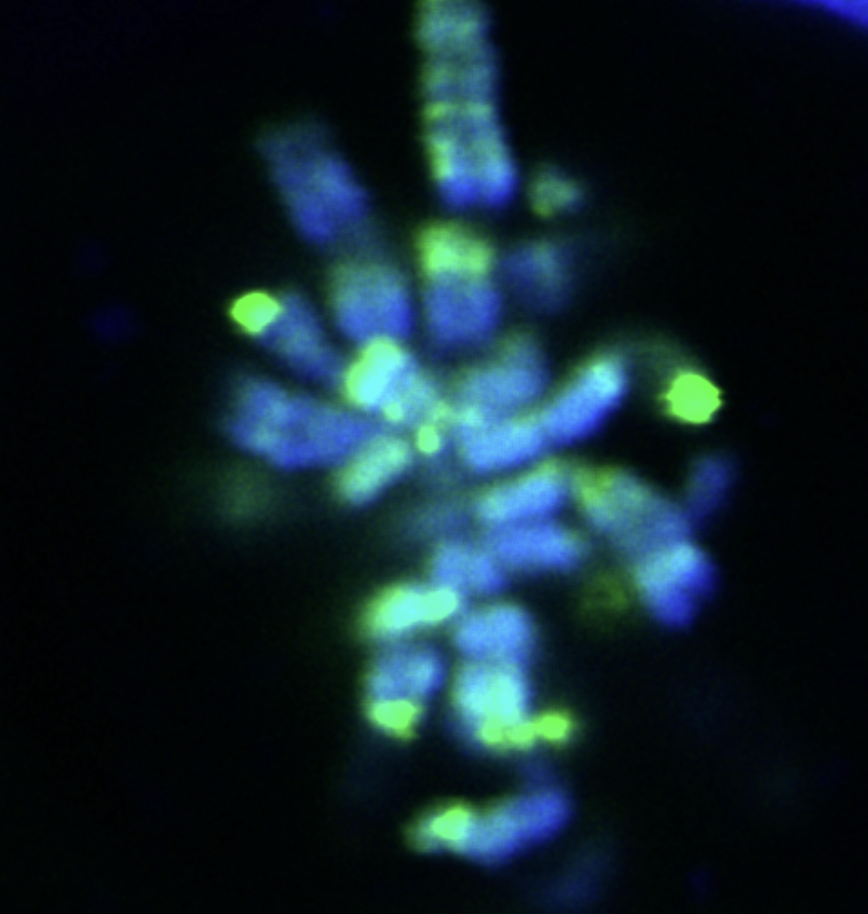
A recurrent theme in sarcoma biology, as well as in many other tumors, is the implication of genes encoding chromatin-modifying activities. Such genes are frequent targets of somatic mutation in cancer and encode for components of the mammalian SWItch/Sucrose Non-Fermentable (SWI/SNF) nucleosome-remodeling complexes and of the Polycomb group (PcG) of proteins. While the former is thought to remodel nucleosomes to facilitate gene accessibility to transcription machinery, PcG proteins selectively repress gene expression via the formation of multi-subunit complexes termed Polycomb repressive complexes (PRCs). The implication of the SWI/SNF subunit, SS18 (translocated in synovial sarcoma) as well as many recent studies revealing alterations in the PRC1.1 complex member – BCOR in several pediatric tumors, further stresses the importance of disturbing normal epigenetic mechanisms in cancer. We continue to understand the role of Polycomb target de-regulation in sarcomas aiming at unraveling common molecular mechanisms of oncogenesis.
Pediatric sarcomas are usually characterized by a low mutational burden. Chromosomal translocations generate oncogenic fusion proteins that act as main cancer drivers. Because they are tumor-specific and thought to play a fundamental role in tumor maintenance, they stand out as perfect hits for targeted therapies. Still, only a few sarcoma oncofusions have been shown to be required for continuous sarcoma cell proliferation in vitro. Moreover, the effect of oncofusion withdrawal in vivo in an immunocompetent background remains mostly unknown. We aim to understand the requirement of various oncogenic gene fusions for tumor maintenance in vitro and in vivo and study mechanisms they regulate that can be explored therapeutically.
Sarcomas are very diverse with more than 50 genetically distinct subtypes and their classification is ever-changing with the rapidly growing molecular classifications. Substantial therapeutic advances are largely lacking due to the difficulty to recapitulate these heterogeneous diseases by conventional model systems. To fill this gap, we are generating an array ofimmunocompetentsarcomamodels based on the electroporation of transposon vectors into the murine muscle (EPO-GEMMs technology). These models are allowing the study of co-operation between genetic alterations, optimization of immunotherapies and to understand mechanisms of tumor maintenance at the single cell level. To aid in clinical translation we are also generating patient-derived xenogfts (PDXs) for pediatric sarcomas.
Benabdallah NS, Dalal V, Sotiriou A, Scott RW, Kommoss FKF, Pejkovska A, Gaspar L, Wagner L, Sánchez-Rivera FJ, Ta M, Thornton S, Nielsen TO, Underhill TM, Banito A. An autoregulatory feedback loop converging on H2A ubiquitination drives synovial sarcoma. (2022) bioRxiv preprint.
Li J, Mulvihill TS, Li L, Barrott JJ, Nelson ML, Wagner L, Lock IC, Pozner A, Lambert SL, Ozenberger BB, Ward MB, Grossmann AH, Liu T, Banito A, Cairns BR and Jones KB. A role for SMARCB1 in synovial sarcomagenesis reveals that SS18-SSX induces canonical BAF destruction. Cancer Discov. (2021), Jun 2. doi: 10.1158/2159-8290.CD-20-1219.
Banito A, Li X, Laporte A, Roe JS, Huang CH, Dancsok A, Tschaharganeh DF, Tasdemir N, Ladanyi M, Jones KB, Capecchi MR, Vakoc CR, Torsten N, Lowe SW. SS18-SSX oncoprotein hijacks KDM2B-PRC1.1 to drive synovial sarcoma. Cancer Cell. (2018) March; 33 (3): 527-541.
- Claudia Winter (Lab manager, TA)
- Dimtry Lupar (Colony manager, TA)
- Nezha Benabdallah, PhD (Postdoc)
- Roland Imle, MD (Postdoc)
- Vineet Dalal, PhD (Postdoc)
- Anastasija Pejkovska (PhD student)
- Afroditi Sotiriou (PhD student)
- Blösel, Daniel (PhD student)
- Clara Gade (MD student)
- Sara Placke (Master student)
- Felix Kommoss (Physician-Scientist)

Postal address:
Junior Research Group Soft-Tissue Sarcoma B380
German Cancer Research Center (DKFZ)
Im Neuenheimer Feld 581 (TP4)
69120 Heidelberg
Germany