The Hopp Children’s Cancer Center Heidelberg (KiTZ) is a joint institution of the German Cancer Research Center (DKFZ), Heidelberg University Hospital (UKHD) and the University of Heidelberg (Uni HD.
In contrast to adult cancers, many bone and soft tissue tumors of childhood and adolescence show fewer, but often more severe, genetic alterations. For example, gene fusion often occurs. In this process, gene segments that are normally far away from each other can be recombined in the body's cells. These newly combined gene segments (so-called fusion genes) can then be used to produce cancer-causing proteins in the cells.
The research team led by Thomas Grünewald, head of a research department at the Hopp Children's Cancer Center Heidelberg (KiTZ) and the German Cancer Research Center (DKFZ) and pathologist at Heidelberg University Hospital (UKHD), and Maximilian Knott of Ludwig Maximilian University Munich (LMU) exploited these gene fusions as highly specific starting points for potential gene therapy strategies.
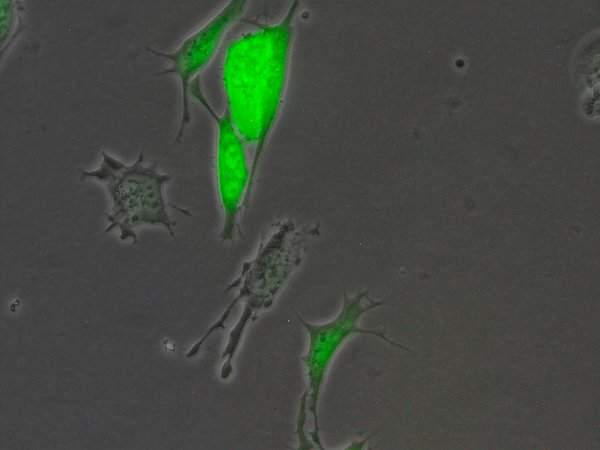
The two fused cancer genes, EWSR1-FLI1 and PAX3-FOXO1, encode novel proteins that can both bind to and activate entirely new DNA segments in tumor cells. This, in turn, turns on genes that help cancer cells proliferate and form metastases in the body. In healthy cells, on the other hand, these regions in the genome are inactive. The fact that these DNA segments are only activated by the fusion genes was used by the scientists for a new gene therapy approach against the tumor cells: Using these target sequences, they constructed a switch that is specifically activated by the fused cancer genes. They combined this switch with a therapeutic gene that alerts the body's immune defenses to the cancer cells and contributes to their destruction. This gene combination was introduced into the cancer cells using lentiviruses. Bone tumor cells with these gene therapy molecules were eliminated, but healthy cells were spared, according to the study of cell cultures in the laboratory and mice.
"Basically, the therapeutic procedure we developed can be called a Trojan horse. We hide a highly effective cancer therapy in a stretch of DNA that tumor cells normally use to drive their proliferation and spread throughout the body. Healthy cells are not hit because they don't have the fused cancer genes needed to turn it on," explains Thomas Grünewald.
The team of scientists now wants to test this therapeutic approach for clinical applicability as soon as possible. "Now the biggest challenge is to target and safely deliver the therapeutic gene segments into a real tumor. The lentiviruses we have used so far as "gene cabs" are not optimal for clinical application. We will therefore focus future studies on bringing the therapy we have developed into more suitable viruses as carriers," adds Maximilian Knott, who coordinated the study at the LMU Institute of Pathology.
It will be several years before the therapy can possibly be used in the clinic. Nevertheless, he says, the foundation has been laid for a completely novel, targeted therapeutic approach that will hopefully soon complement current treatment options.
The study was supported by the Dr. Rolf M. Schwiete Foundation in Mannheim, the German Cancer Aid, and the Association for the Promotion of Science and Research at the Medical Faculty of LMU Munich.