The “Hopp Children's Cancer Center Heidelberg” (KiTZ) is a joint institution of the German Cancer Research Center (DKFZ), Heidelberg University Hospital (UKHD) and Heidelberg University.
Medulloblastoma, malignant tumors in the cerebellum, account for only around one percent of all brain tumors in adults, but are the most common form of malignant brain tumor in children. The medulloblastoma spread from the cerebellum to the surrounding tissue and can also spread to other parts of the central nervous system via the cerebrospinal fluid. Because these tumors grow rapidly, physicians do not have much time to find a suitable treatment.
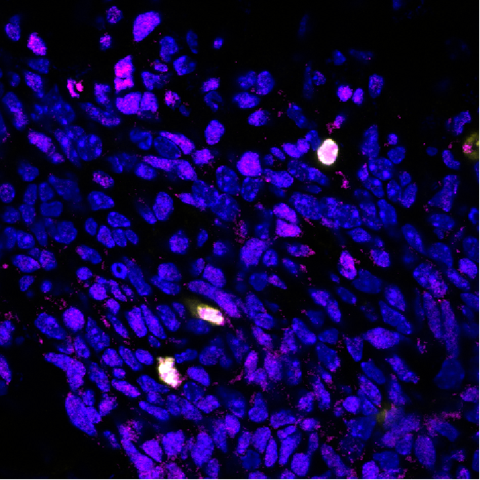
At the Hopp Children’s Cancer Center Heidelberg (KiTZ), scientists are conducting intensive research into the onset of medulloblastoma in order to develop new therapy options. “The onset of malignant medulloblastoma cells has genetic causes and follows several stages,” explains Lena Kutscher, a Junior Group Leader at the KiTZ and the DKFZ. “First, genetic mutations cause excessive proliferation of certain precursor nerve cells, and growths develop. If more mutations occur, they can turn into malignant tumor cells that spread into the surrounding tissue.”
Together with colleagues from the National Institute of Neuroscience in Tokyo and from St. Jude Children’s Hospital in the USA, the research team came across two key genetic drivers for the onset of medulloblastoma in the Sonic Hedgehog medulloblastoma subgroup (SHH). The BCOR gene is regarded as a tumor suppressor gene, and its protein product normally suppresses the uncontrolled division of cells with genetic defects, thereby preventing the onset of tumors. Earlier studies have shown that in eight percent of young SHH patients, BCOR is mutated or has been partially deleted from the genome. Boys are particularly affected by this mutation.
In combination with another gene defect, the loss of the Ptch1 receptor gene, the defective BCOR protein then becomes a key trigger for the onset of brain tumors in mice: mice that were unable to produce both proteins properly developed tumors in all cases. The researchers suspect that the cause is misregulation of the growth hormone Igf2. They found that, both in mice and in some human SHH tumors with defective BCOR protein, Igf2, a gene known to be associated with cancer, was particularly active.
“Our study uncovered a key signaling pathway for the onset of cancer – one that is caused by BCOR mutations in SHH medulloblastoma,” says Daisuke Kawauchi, the last author of the paper, who was previously a group leader at the KiTZ and the DKFZ and is now a research group leader at the National Institute of Neuroscience in Tokyo. “These findings open up new opportunities to develop personalized treatment strategies for patients with and without these genetic mutations.”
Original Publication:
L. M. Kutscher et al. Functional loss of a noncanonical BCOR– PRC1.1 complex accelerates SHH-driven medulloblastoma formation. In: Genes and Development (Online Publication 20. August 2020). DOI: 10.1101/gad.337584.120.
Press contact:
Dr. Alexandra Moosmann
Hopp-Kindertumorzentrum Heidelberg (KiTZ)
Referentin Presse- und Öffentlichkeitsarbeit
Im Neuenheimer Feld 130.3
D-69120 Heidelberg
T: +49 (0) 6221 56 36434
E-Mail: a.moosmann[at]kitz-heidelberg.de
E-Mail: presse[at]kitz-heidelberg.de