The Hopp Children’s Cancer Center Heidelberg (KiTZ) is a joint institution of the German Cancer Research Center (DKFZ), University Hospital Heidelberg (UKHD) and the University of Heidelberg (Uni HD).
Neuroblastomas are the second most common form of solid tumor found in children, after brain tumors. The tumors develop from immature precursor cells of the nervous system and occur in the adrenal glands, or along the spine – in the neck, chest or abdomen. In some cases, neuroblastomas shrink and completely disappear without any therapy at all. But in around half of all patients, even highly intensive treatment is unable to prevent the tumor from growing.
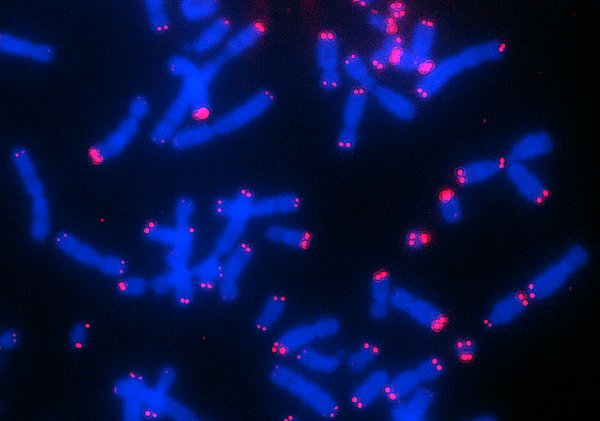
Malignant neuroblastoma cells employ a trick so that they can carry on dividing: they lengthen their telomeres, the caps at the end of their chromosomes. In healthy body cells, the telomeres are shortened with every cell division. Once a critical length is reached, telomer shrinkage leads to growth stoppage or cell death. By contrast, in stem cells and most cancer cells, the length of the telomeres is kept above the critical threshold by means of lengthening mechanisms, making the cells practically ‘immortal’.
“The cancer cells do this in one of two ways at the molecular level,” explains Sabine Hartlieb from the KiTZ, the DKFZ and the University of Heidelberg, who is one of the two lead authors of the paper. “They either overactivate the telomerase enzyme, which also keeps the telomere length as constant as possible during cell division in healthy stem cells, for instance. Or they lengthen the shortened chromosome ends by rearranging their telomere segments.” This latter mechanism is what scientists call the alternative lengthening of telomeres. “Tumors in which telomere lengthening is activated, by either of these methods, all have a poor prognosis,” says Frank Westermann, who was leading the study at the KiTZ and the DKFZ.
This is confirmed by the data from 760 neuroblastoma patients in the study. However, in nearly half of the patients who suffered a relapse, it was not overactivation of telomerase, but the alternative lengthening of telomeres that was responsible.
By integrating genetic and epigenetic data and the first ever analysis of all the proteins present in the tumor, the scientists investigated which molecular processes promote this specific lengthening mechanism. Summarizing the results, Lina Sieverling, one of the two lead authors, who works at the DKFZ and the NCT in Heidelberg, says, “Tumors with this telomere lengthening mechanism differ significantly from other neuroblastoma subgroups in terms of certain mutations, protein complexes and epigenetic signals.” For instance, the study found that malignant neuroblastoma have methylation signals on their protein histone 3 in the telomere region. This packages DNA into chromosomes, giving them a particularly compact and stable structure. Numerous other proteins from these tumors also showed characteristic modifications that were only partially visible, if it all, at genetic level. Scientists have long known that changes to the ATRX gene are associated with the alternative mechanism. Now they have been able to show that the ATRX/DAXX protein complex is modified in all tumors of this subgroup, even in cases where there was no discernible genetic mutation.
“These clear molecular differences are also reflected in the different clinical course of the disease in this group of patients,” stresses Frank Westermann. “Until now, all these young patients have been treated with the same chemotherapy protocols, which primarily attack fast-growing cancer cells. However, cancer cells with the alternative mechanism tend to grow slowly, but keep on growing, and are extremely resilient. We are dealing here with constantly recurring tumors, for which these standard therapies are very probably not the best solution,” says Westermann. “In the next stage, we will work on developing a specific therapy for these tumors because these children urgently need new treatment concepts. And such concepts could presumably also be used to treat other types of cancer that make use of the same special telomere lengthening mechanism.”
Original publication:
S. A. Hartlieb, L. Sieverling et al. Alternative lengthening of telomeres in childhood neuroblastoma from genome to proteome. In: Nature Communications (online publication 24th 2021). DOI: 10.1038/s41467-021-21247-8
Press contact:
Dr. Alexandra Moosmann
Hopp-Kindertumorzentrum Heidelberg (KiTZ)
Referentin Presse- und Öffentlichkeitsarbeit
Im Neuenheimer Feld 130.3
D-69120 Heidelberg
T: +49 (0) 6221 56 36434
E-Mail: a.moosmann[at]kitz-heidelberg.de
E-Mail: presse[at]kitz-heidelberg.de