Pediatric Immuno-Oncology
Our junior research group investigates new immunotherapies for the treatment of childhood cancers.
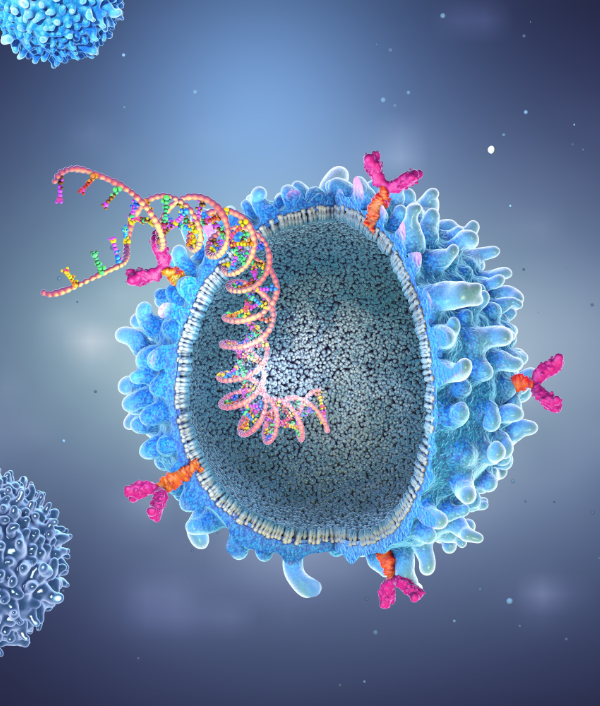
Our immune system is not only capable of fighting infections but can also, in principle, recognize and eliminate cancer cells. The principle of immunotherapy involves "training" the immune system to fight cancer. This is achieved, for example, through genetic modification of specific immune cells called T cells. These T cells can be engineered to carry a chimeric antigen receptor (CAR) on their surface. The resulting CAR T cells can then recognize and eliminate cancer cells in the patient’s body.
This type of therapy has already been highly successful in treating children and adolescents with a specific type of blood cancer (lymphoblastic leukemia). Unfortunately, the therapy has so far been less effective for other forms of blood cancer (myeloid leukemia) and most solid tumors (e.g., brain tumors or bone tumors). We aim to change this. Our research projects focus on questions such as: What strategies have tumors developed to evade detection by the immune system? How can CAR T cells recruit other immune cells for help? How can we optimize T cells to effectively migrate to solid tumors and eliminate them?
-
Immunotherapy with genetically modified T cells
How can we develop more effective CAR T cell therapies for children with cancer? Together with other KiTZ teams, we are working to identify new target structures on pediatric tumors, including malignant brain cancers. Based on these discoveries, we are designing novel CAR T cell therapies with the goal of creating safer and more effective treatments for children in the future.
-
Immune cell interactions in solid tumors
How do CAR T cells communicate with tumor cells and with other immune cells? To answer this, we use advanced spatial technologies and specialized labeling methods to visualize these interactions within the tumor environment. Our goal is to understand how CAR T cells behave in solid tumors and how we can optimize their ability to coordinate and strengthen an anti-tumor immune response.
-
CRISPR screens and genetic engineering
In recent years, many new tools for T cell engineering have emerged, such as CRISPR cutting, CRISPRa, CRISPR knock-in, base editing, and prime editing. In our lab, we not only use these technologies but also refine and adapt them for large-scale CRISPR screens. This enables us to test hundreds to thousands of CAR T cell modifications in parallel—an approach that significantly accelerates the discovery of promising new therapies (see Spotlight section).
-
Understanding resistance to immunotherapies
Why are immunotherapies like CAR T cells highly effective in some cancers (such as lymphoblastic leukemia) but show little benefit in others (such as myeloid leukemia)? To answer this question, we are applying genome-wide CRISPR screens to uncover the mechanisms that are causing resistance in some malignancies. At the same time, we are developing new immunotherapy strategies designed to overcome these barriers and expand the success of CAR T cell therapy to a broader range of cancers.
Blaeschke, F., Chen, Y., Apathy, R., Daniel, B., Chen, A.Y., Chen, P., Sandor, K., Zhang, W., Li, Z., Mowery, C.T., Yamamoto, T.N., Nyberg, W.A., To, A., Yu, R., Bueno, R., Kim, M., Schmidt, R., Goodman, D.B., Feuchtinger, T., Eyquem, J., Ye, C.J., Carnevale, J., Satpathy, A.T., Shifrut, E., Roth, T.L., and Marson, A. (2023). Modular Pooled Discovery of Synthetic Knockin Sequences to Program Durable Cell Therapies. Cell 186, 4216-4234 e4233.
Carnevale, J., Shifrut, E., Kale, N., Nyberg, W.A., Blaeschke, F., Chen, Y.Y., Li, Z., Bapat, S.P., Diolaiti, M.E., O'leary, P., Vedova, S., Belk, J., Daniel, B., Roth, T.L., Bachl, S., Anido, A.A., Prinzing, B., Ibanez-Vega, J., Lange, S., Haydar, D., Luetke-Eversloh, M., Born-Bony, M., Hegde, B., Kogan, S., Feuchtinger, T., Okada, H., Satpathy, A.T., Shannon, K., Gottschalk, S., Eyquem, J., Krenciute, G., Ashworth, A., and Marson, A. (2022). RASA2 ablation in T cells boosts antigen sensitivity and long-term function. Nature 609, 174-182.
Schmidt, R., Steinhart, Z., Layeghi, M., Freimer, J.W., Bueno, R., Nguyen, V.Q., Blaeschke, F., Ye, C.J., and Marson, A. (2022). CRISPR activation and interference screens decode stimulation responses in primary human T cells. Science 375, eabj4008
Blaeschke, F., Stenger, D., Apfelbeck, A., Cadilha, B.L., Benmebarek, M.R., Mahdawi, J., Ortner, E., Lepenies, M., Habjan, N., Rataj, F., Willier, S., Kaeuferle, T., Majzner, R.G., Busch, D.H., Kobold, S., and Feuchtinger, T. (2021). Augmenting anti-CD19 and anti-CD22 CAR T-cell function using PD-1-CD28 checkpoint fusion proteins. Blood Cancer J 11, 108.
- Dr. Dr. Franziska Blaeschke (Group leader)
- Dr. Oren Barboy (Postdoc)
- Dr. Caroline Fandrey (Postdoc)
- Maria Gruber (Student assistant)
- Kathleen Grüter (PhD student)
- Lara Kellendonk (Student assistant)
- Monika Kuban (Lab manager)
- Konstantin Loher (PhD student)
- Jan Reichert (Intern/MD student)

Postal address:
Hopp Children's Cancer Center Heidelberg
Im Neuenheimer Feld 280
D-69120 Heidelberg
Germany