Spotlight - JRG Deng
Road from molecular brain tumor classification to personalized radiation treatment planning
The landscape of neuro-oncology has undergone a transformative shift with the advent of molecular brain tumor classification. Traditional histopathological methods, which relied heavily on microscopic examination of tumor morphology, often fell short in capturing the biological diversity and clinical behavior of brain tumors. The integration of genomic and molecular profiling into diagnostic practices has revolutionized our understanding of these tumors, revealing a complex tapestry of genetic alterations that underpin distinct molecular subgroups.
Molecular classification has provided deeper insights into the pathogenesis of brain tumors, allowing for the identification of novel biomarkers and therapeutic targets. This paradigm shift from a morphology-based to a molecular-based classification has paved the way for more individualized treatment approaches.
Radiation therapy represents a cornerstone in the management of brain tumors. Personalized radiation treatment planning, informed by molecular profiles, may optimize therapeutic outcomes by tailoring radiation doses and target volumes to the specific molecular risk profile of the tumor. Furthermore, the integration of molecular data into radiation oncology may enable the development of advanced imaging techniques and computational models that predict tumor response and potential radiation-induced damage to surrounding healthy tissues.
The translation from molecular brain tumor classification to personalized radiation treatment planning requires a multidisciplinary approach, combining the expertise of molecular biologists, pathologists, radiologists, and radiation oncologists to deliver a tailored and effective radiation treatment. As we continue to unravel the molecular complexities of brain tumors, the potential for personalized radiation therapy to improve patient outcomes becomes increasingly attainable, which may mark a significant advancement in the fight against brain cancer.
Deng M et al. Clinical outcome following surgical resection and radiotherapy in adult patients with pleomorphic xanthoastrocytoma as defined by DNA methylation profiling. Neurooncol Pract. 2023 Jan 18;10(3):307-314. doi: 10.1093/nop/npad004. PMID: 37188167; PMCID: PMC10180362.
Integrated analysis of preoperative and post-therapeutic MR-imaging and radiation treatment plans in molecularly defined pleomorphic xanthoastrocytoma
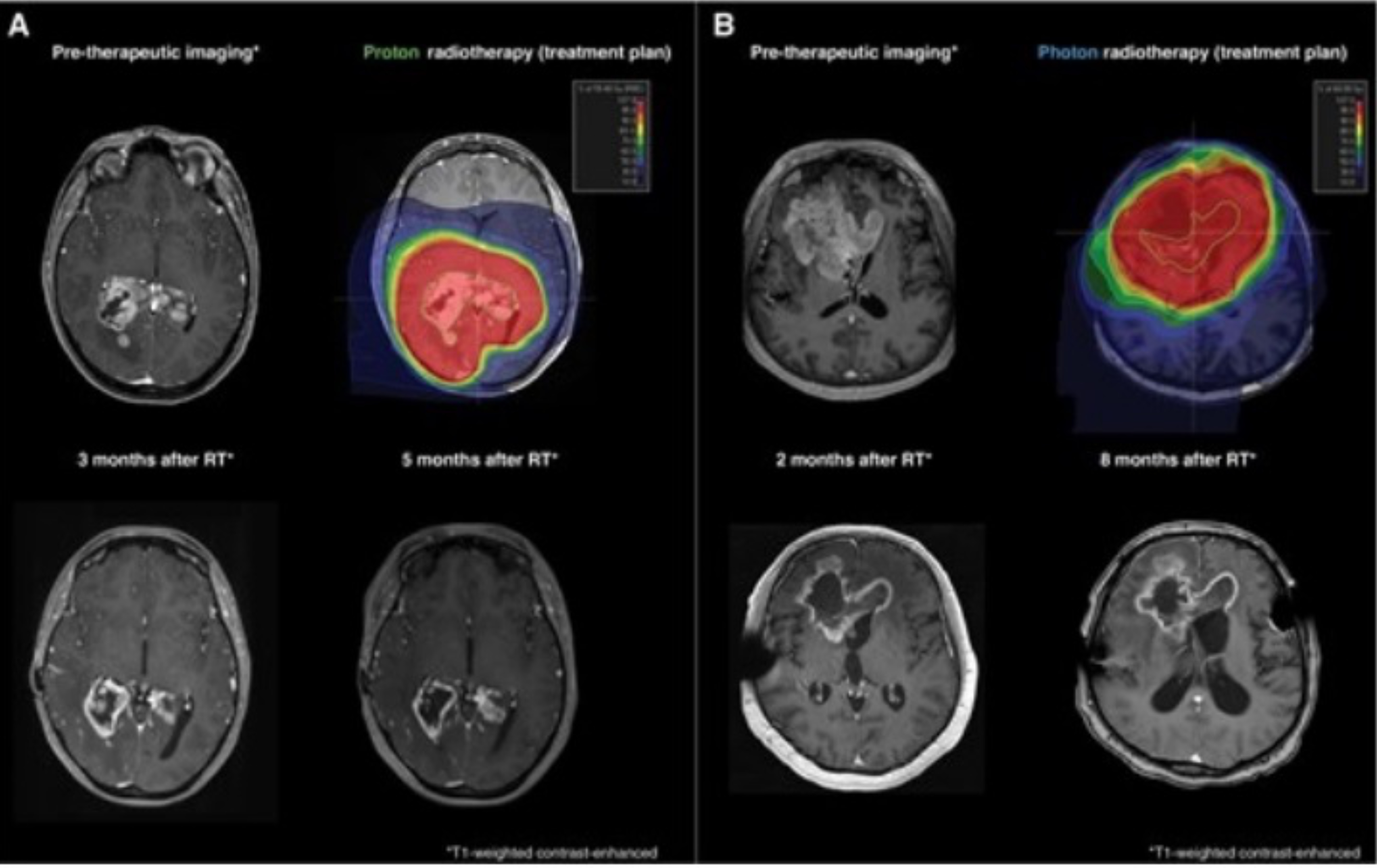
(A) Proton therapy with a total dose of 59.4 Gy (RBE) in 33 fractions was administered following tumor biopsy. Follow-up imaging demonstrated a partial response in 3- and 5-months following radiotherapy, according to RANO guidelines. (B) Photon radiotherapy with 60 Gy in 30 fractions was applied following subtotal resection. Follow-up imaging demonstrated a stable disease in 2- and 8-months following radiotherapy, according to RANO guidelines. PTVs are depicted in blue, CTVs in red and GTVs in green.

